Text “BABY” to 511411
Get FREE tips on your cell phone to help you through your first pregnancy and your baby’s first year.
Powered by Voxiva.
Text4baby is a program of the National Healthy Mothers, Healthy Babies Coalition.
Text “BABY” to 511411
Get FREE tips on your cell phone to help you through your first pregnancy and your baby’s first year.
Powered by Voxiva.
Text4baby is a program of the National Healthy Mothers, Healthy Babies Coalition.
REAR FACING CAR SEAT

FORWARD FACING CAR SEAT

BOOSTER SEAT

SEAT BELT

ALL children younger than age 13 should ride properly restrained in the back seat.
NEVER place a car seat in the front passenger seat.
For additional information and assistance contact EMS Car Safety Checks and Infant Safety Education at 512-972-7233 or www.atcems.org.
For other car seat check option call Dell Children’s Medical Center 512-324-8687 or Safe Riders 1-800-252-8255.
Never leave a child alone in a car!
WHAT IS COLIC?

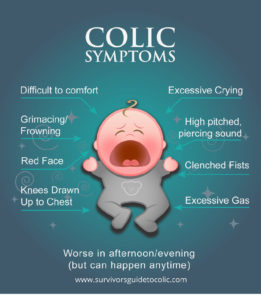
SYMPTOMS:
REMEMBER
There is no cure for colic and there is no known cause, but there are ways to help.
THINGS TO TRY:



IF NOTHING WORKS:
Source: TexasWIC.org
Get To Know Your New Baby: WIC’s Guide for Birth to 3 Months
A New Baby!
You must feel excited and completely overwhelmed!
This booklet will help you learn what your newborn needs to be happy and healthy.
All babies are different, but their movements and noises will let you know when they’re hungry, happy, uncomfortable or just tired.
You will soon learn your baby’s cues and become your newborn’s superhero!
– 1 cup of warm water
– Kitchen Measuring Spoons
– Table Salt
– Nose Dropper
– Bulb Syringe
– Soft Tissues
– A Soft Rolled Up Blanket or Towel
To make the mucous more watery, add saline (salt) water in the nose. To make the salt water drops:
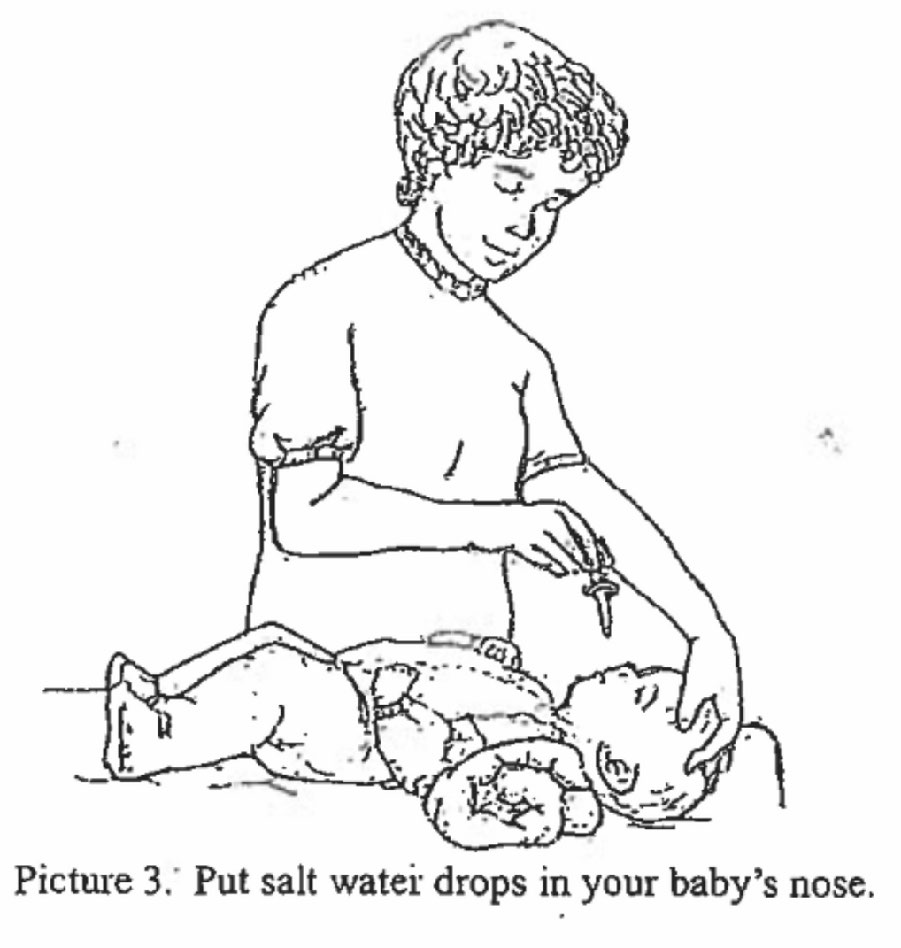

1. Suction your baby before you feed her. If you suction after, the salt water might cause vomiting.
2. To use the bulb syringe, squeeze the air out of the bulb as shown in Picture 4 (above).
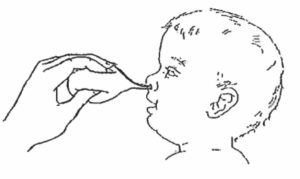
3. While squeezing, gently put the tip of the bulb into on nostril as demonstrated in picture 5 (below).
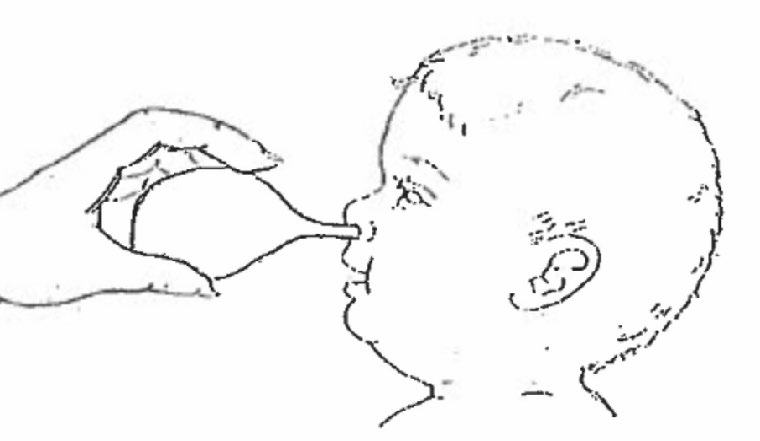
4. Stop squeezing to let the air come back into the bulb. This will pull the mucous out as shown in Picture 6 (above).
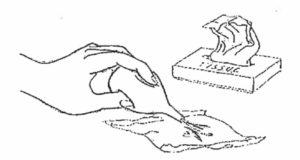
5. Squeeze the mucous out of the bulb onto a tissue as shown in Picture 7 (below).
6. Suction the other nostril the same way.
1. Gently wipe off the mucous around the baby’s nose with tissues.
2. Wash the cup, the dropper, and the bulb syringe in warm soapy water.
3. Squeeze the bulb syringe several times to clean out the mucous. Rinse with clean water.
WHAT IS JAUNDICE?

The newborn on the left does not have jaundice as a yellowish tint is absent.

The newborn on the right has jaundice as seen from the yellowish tint of the skin and eyes.
CAN JAUNDICE HURT MY BABY?
WHAT CAN I DO TO HELP MY BABY’S JAUNDICE GO AWAY?
DOES BREASTFEEDING AFFECT JAUNDICE?
During the COVID-19 pandemic, parents may need to check their children for symptoms, including fever, before they go to school, child care, or sports activities. Feeling your child’s forehead is quick but not very exact. Most modern digital thermometers work fast and are easy to use.
A “normal” temperature varies with the child’s age, activity, and time of day. A fever usually is a temperature of 100.4 degrees Fahrenheit (38 degrees Celsius) or higher. This is a sign that the body is fighting an illness. Your child’s temperature, age and other signs of illness will help your doctor recommend treatment that is best for your child.
Call your pediatrician right away if your child:
What are some different types of digital thermometers?
There are different types of digital thermometers that measure temperature at different areas of the body. Rectal (in the anus) temperatures are the most accurate. Forehead temperatures are the next most accurate. Oral and ear temperatures are accurate if done properly. Armpit temperatures are the least accurate, but you can use this method to screen a child of any age.
Whatever approach is used, follow the cleaning instructions on the package before use.



How to Use a Digital Thermometer
To get the right thermometer reading, it is important to always follow the instructions that came with the device.
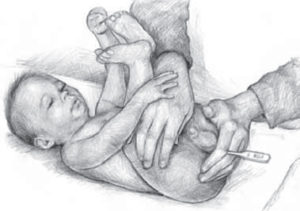
Rectal temperature
Taking a rectal temperature gives the best reading, especially for infants under 3 months of age. Here is how to take a rectal temperature:
Oral temperature
 Once your child is 4 years old, you can take a temperature by mouth. Here is how to take an oral temperature:
Once your child is 4 years old, you can take a temperature by mouth. Here is how to take an oral temperature:
Forehead temperature
Temporal artery (forehead) thermometers can be used on children of any age. Here is how to take a forehead temperature:
Ear temperature
Tympanic (ear) thermometers can be used on children 6 months of age and older, as young infants have narrow ear canals. Here is how to take an ear temperature:
Some quick screening ways may not be best
Some products and quick methods are not as accurate at checking a child’s temperature. For example, taking the temperature under the armpit can help schools and child care centers quickly check, but is not very accurate.
Other less accurate ways of checking for fever include using a pacifier thermometer (for children 1 year of age and younger) and fever strips on the forehead. While parents can use them for quick screening, they do not work as well as measuring your child’s rectal, forehead, ear, or oral temperature with a digital thermometer.
Remember
Fever is just one sign of illness, but an important one. Talk with your child’s pediatrician if you have any questions about fever and taking your child’s temperature.
More Information
*Digital thermometer drawings by Anthony Alex LeTourneau.
Last Updated: 10/12/2020
Source: American Academy of Pediatrics (Copyright © 2020)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.